Abstract
Introduction: Mutations and deletions in TP53 are found in all hematological malignancies, Whereas TP53 mutations (TP53mut) were described to occur quite frequently in acute lymphocytic leukemia (ALL). Previous studies have demonstrated that TP53 mutation was associated with poor prognosis in ALL. Allogeneic hematopoietic stem cell transplantation (HSCT) represents an effective therapy for reducing the chances of relapse of ALL. Recent medical progress has led to haploidentical-SCT (haplo-SCT) achieving transplant outcomes similar to those with matched-sibling donor SCT and matched-unrelated donor SCT in patients with hematological malignancies, haplo-SCT provided an alternative treatment for ALL patients for whom identical donors are unavailable. However, the impact of TP53mut in ALL on survival outcomes in haplo-HSCT setting remains unknown. This study aims to investigate the effect of TP53 mutations on survival outcomes of ALL treated with haplo-SCT at a single institution.
Methods: 78 subjects with available TP53 status at diagnosis were retrospectively considered. We excluded 11 subjects who received HLA-matched related transplantation and 2 subjects with HLA-matched unrelated donor transplantation. The remaining 65 subjects with haplo-HSCT were enrolled. TP53 mutation analysis was assessed on bone marrow (BM) samples. LFS and OS were estimated using Kaplan and Meier method and tested between groups using a log-rank test. Cumulative incidence of relapse (CIR) was treated as a competing risk for non-relapse mortality (NRM).
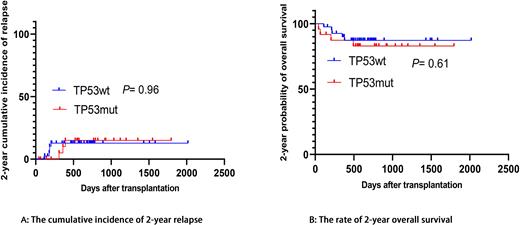
Results: A cohort of 65 patients was included with a median(range) age of 30 years (14-51) and was followed up for a median duration of 602 days (range;42-2017 days). 60% of patients were male. 24 of 65 patients showed TP53 mutations. The baseline characteristics including sex, age, white blood cell, diagnosis, Ph/Ph-like chromosomes, IKZF1 mutation, donor-recipient gender, donor-recipient relation, ABO mismatched, CR status before SCT, pre-MRD status were similar between the two groups. 7 (10.8%) patients suffered platelet engraftment failure, the cumulative incidence of grade II-IV aGVHD or cGVHD was comparable between the two groups (TP53mutvs TP53wt:38.8% vs 30.2%, P=0.80; 69.0% vs 63.4%, P=0.98). The 2-year cumulative of CIR rates were 13.1% and 12.5% (P=0.96) among TP53mut and TP53wt patients. The 2-year LFS rates of TP53mut patients were similar to patients with TP53wt (74.2% vs 77.4%, P=0.80). No significant differences in 2-year OS rates (82.9% vs 87.3%, P=0.61) or 2-year NRM rates (12.7% VS 10.2%, P=0.69) were observed in TP53mut and TP53wt patients. TP53 played no prognostic role in multivariate analysis. WBC count at diagnosis (>50x109/L: HR=3.860, P=0.016) and age (>40 years old: HR=4.120, P=0.012) were independent risk factors associated with 2-year LFS, additionally, cGVHD showed protective effect for 2-year LFS in univariate analysis (P= 0.06), but significant was not confirmed in a multivariate analysis. WBC count at diagnosis (>50 x109/L: HR=5.483, P=0.042) was the only independent risk factor of 2-year CIR. To assess the prognostic impact of TP53mut in a homogeneous population, we reanalyzed patients with B-cell immunophenotype. There was no significant difference in survival outcomes between TP53mut and TP53wt groups when only B-ALL were assessed (TP53mutvs TP53wt: 2-year OS: 82.2% vs 93.0%, P=0.23; 2-year LFS: 73.0% VS 82.7%, P=0.44; 2-year NRM:13.3% vs 7.1%, P=0.40; 2-year CIR:13.7% vs 10.2%, P=0.81).
Conclusion: Our study showed that TP53 mutations may not be related to the unfavorable impact on survival in ALL patients after treatment with haplo-HSCT. The results imply that haplo-HSCT may be a viable treatment for this subgroup of patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal